Lab color readings
4.4 Lab Colour Space and Delta E Measurements – Graphic Design and Print Production Fundamentals
Chapter 4. Colour Management in the Graphic Technologies
Alan Martin
The CIE (Commission Internationale d’Eclairage or International Commission on Light) is a scientific body formed by colour scientists in the 1930s that has provided much of the fundamental colour knowledge we possess today. Three core definitions provided by the CIE are the standard observer, the Lab colour space, and Delta E measurements. The latter two are particularly important for colour management.
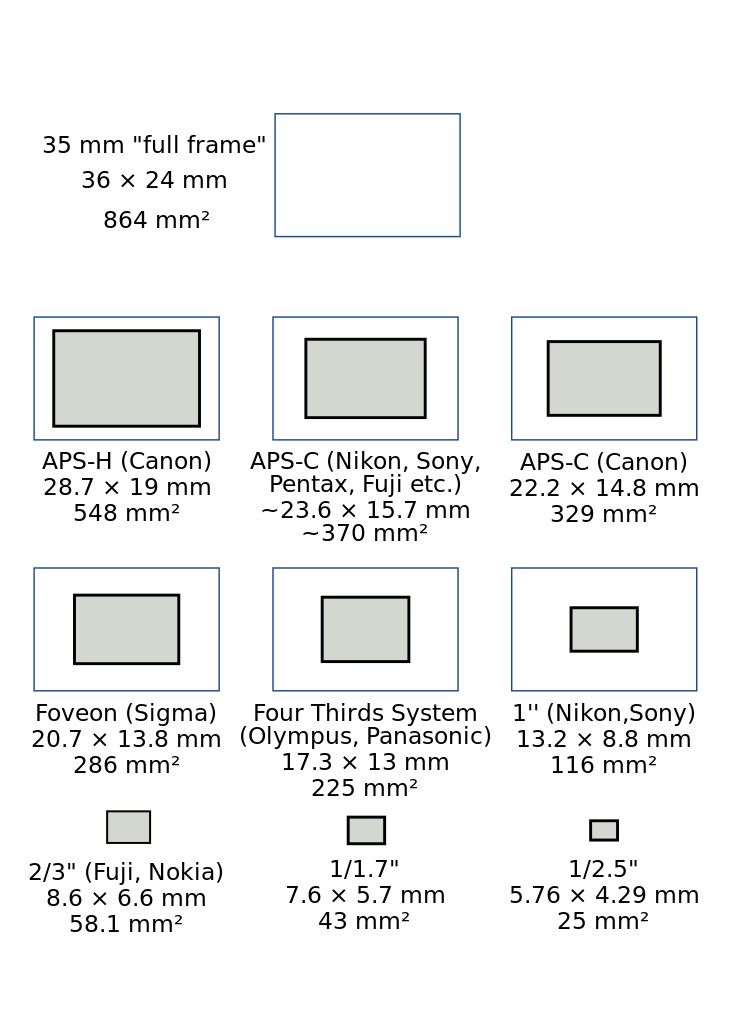
In section, 4.2, we mentioned the Lab colour space as a natural outgrowth of understanding the function of opponency in human vision. It’s comprised of three axes: L represents darkness to lightness, with values ranging from 0 to 100; a represents greenness to redness with values of -128 to +127; and b represents blueness to yellowness also with values from -128 to +127.
Notice that there are no negative values on the L axis as we can’t have less than zero light, which describes absolute darkness. The L axis is considered meaning without colour. Here we are dealing with the volume rather than the kind of light. In contrast, the a and b axes are , describing the colour character and the type of light.
The standard two-dimensional depiction is of only the a and b axes, with a as the horizontal axis and b as the vertical axis. This places red to the right, green to the left, blue at the bottom, and yellow at the top. If you found our previous mnemonic aid of POLO helpful, you can use RGBY to remember the colour pairs. For correct placement, remember that red is on the right, and blue is on the bottom.
Colours are more neutral and grey toward the centre of the colour space, along the L axis. Imagine that equivalent values of the opposing colours are cancelling each other out, reducing the saturation and intensity of those colours. The most saturated colours are at the extremes of the a and b axes, in both the large positive and negative numbers. For a visual depiction of the Lab colour space, open the ColorSync application found in the Utilities folder of any Macintosh computer and view one of the default profiles such as Adobe RGB.
The most saturated colours are at the extremes of the a and b axes, in both the large positive and negative numbers. For a visual depiction of the Lab colour space, open the ColorSync application found in the Utilities folder of any Macintosh computer and view one of the default profiles such as Adobe RGB.
Now it’s time to explore the practical application of this colour map for the comparative analysis of colour samples. We can’t make any progress in evaluating our success in colour matching unless we have a frame of reference, some yardstick to determine how much one colour sample is similar or different from another. That yardstick is the Delta E measurement.
Figure 4.7 Lab Colour SpaceDelta, the fourth letter of the Greek alphabet and symbolized as a triangle, is used in science to indicate difference. is the difference between two colours designated as two points in the Lab colour space. With values assigned to each of the L, a, and b attributes of two colours, we can use simple geometry to calculate the distance between their two placements in the Lab colour space (see Figure 4. 7).
7).
How do we do that? It looks a lot like the formula used to determine the long side of a right triangle that you may remember from high school geometry. We square the difference between each of the L, a, and b values; add them all together; and take the square root of that sum. Written out as a formula it looks a little more daunting: .
Let’s try a simple example to see what we get. Colour 1 has a Lab value of 51, 2, 2 and Colour 2 is 50, 0, 0 (right at the centre of the colour space):
, and, so our first value is 1.
; and , so our second value is 4.
, so the third value is also 4.
Add them together: ; and take the square root: .
The Delta E (difference) between our two colours is 3. Could we detect that difference if we were viewing those two colours? Probably just barely. The minimum Delta E for seeing a difference is about 2. Smaller differences can normally be detected in neutral colours (such as our samples), while more saturated colours require a slightly larger Delta E. A Delta E of 4 is the upper threshold for acceptable machine repeatability or consistency.
A Delta E of 4 is the upper threshold for acceptable machine repeatability or consistency.
Delta E provides a value indicating the overall difference between two colours. It does not provide any colour-related data such as which colour is lighter/darker, redder/greener, more blue/more yellow. To understand how the colours are different, we have to evaluate the comparative L, a, and b differences independently.
Experimentation over time has come to show that conventional Delta E is about 75% accurate in showing the difference we see between two colours. Delta E numbers exaggerate the differences in yellows and compress our perceptual distance between blues. To improve on the representation of our interpretation of colour difference, scientists have produced a modified formula known as Delta E(94).
Delta E(94) is a modified formula that provides about 95% accuracy in correlation to human perception of colour differences. Here it is in all its splendour:
where:
(for reference conditions)
You can see that it is still the comparison of three values: L, C, and H, where C and H are produced by applying modifying factors to the original Lab values to compensate for perceptual distortions in the colour space. Each difference is squared and the root taken of the sum of the squares, just as in the original Delta E formula.
Each difference is squared and the root taken of the sum of the squares, just as in the original Delta E formula.
There is an additional refinement in Delta E(2000) where further adjustments are applied to blue and neutral colours and compensations for lightness, chroma, and hue. This is a much smaller correction than the change from Delta E to Delta E(94).
The good news is that you don’t need to understand or remember any of the details of these equations. Just remember that these are real numbers measuring actual plotted distances between colour samples. Delta E represents the distance between two points in the Lab colour space. Delta E(94) and Delta E(2000) are enhancements, providing improved numbers that more closely match our perception of colour differences.
Media Attributions
- Delta E in Lab Colour Space © Ken Jeffrey
The CIELAB L*a*b* System – the Method to Quantify Colors of Coatings
Share this article:
Introduction
Color is an important aesthetic aspect of coated objects. Different persons have different perceptions of a specific color. Therefore, it is important to have an objective way to characterize colors of coatings, as well as to quantify differences between colors. The good news is that there is a standard system that is used all over the globe: the CIELAB color system. This article is about the fundamentals of this system.
Different persons have different perceptions of a specific color. Therefore, it is important to have an objective way to characterize colors of coatings, as well as to quantify differences between colors. The good news is that there is a standard system that is used all over the globe: the CIELAB color system. This article is about the fundamentals of this system.
The CIELAB Color Space
The 3-dimensional CIELAB color spaceThe color of (coated) objects is visualized and quantified by using the CIELAB color space. The 3-dimensional color space is built-up from three axes that are perpendicular to one another.
The L*-axis gives the lightness: a white object has an L* value of 100 and the L* value of a black object is 0. The so-called achromatic colors, the shades of grey, are on the L*-axis.
Chromatic (‘real’) colors are described by using the two axes in the horizontal plane. The a*-axis is the green-red axis and the b*-axis goes from blue (-b*) to yellow (+b*).
The a*-axis is the green-red axis and the b*-axis goes from blue (-b*) to yellow (+b*).
Each color is represented by a color point (L*, a*, b*) in the color space; L*, a* and b* are the color coordinates of the color point.
The asterisk (*) symbol of L*, a* and b* indicates that this is the new color system; it is the follow-up of the older CIELAB system. The new system is now universally used for the quantification of colors, even though often the simplified notation of the Lab-values, without the * symbol, is used.
Color differences
The color difference between two colors is the distance between the color points of the two colors. ΔE*ab is the color difference of two colors, ‘1‘ and ‘2’, that have color coordinates L*1, a*1, b*1 and L*2, a*2, b*2, respectively. A small ΔE*ab value implies that the colors are close to one another. The color difference can be calculated by using the mathematical theorem of Pythagoras:
A small ΔE*ab value implies that the colors are close to one another. The color difference can be calculated by using the mathematical theorem of Pythagoras:
The concept and quantification of color differences is important when a color must be matched or when a new batch of a paint must have a color that is close to the color of the standard paint, the reference. But, how well must the color of the new batch match with the color of the reference? The answer to this question is a criterion in the quality control of a new batch of paint. The color coordinates of the batch and the reference are measured and the color difference ΔE*ab is calculated. Depending on the industry, the criterion for color approval can be strict, for example ΔE*ab < 0.3, or much milder, for example ΔE*ab < 1.5.
In the daily practice of those who work with paints, the representation of a color difference is often simplified as ΔE* or ΔE.
Hue and Chroma
Hue is the color tone or color name of a color. Chroma is the amount of saturation of a color. Colors of high chroma are said to be clear, bright or brilliant. Dull (pastel) colors have a low chroma.
Hue and chroma can be visualized and quantified by using the a*b*-plane of the CIELAB color space.
Hue angle and chroma in the a*b*-planeThe hue of a color is quantified by its hue angle hab (without * symbol) in the a*b*-plane, given in degrees (°). The hue angle range starts, by definition, at the positive side of the a*-axis and goes counter-clockwise. This implies that red has a hue angle of 0°. A full circle goes from 0° to 360°. Cyan blue (an organic blue pigment with color index PB 15), for example, has a hue angle of about 240°. The hue angle of a color can be calculated from the color coordinates:
The chroma of a color is quantified by C*ab; it is the distance of the color point to the L*-axis. Chroma can be calculated from the color coordinates by using Pythagoras’ theorem:
Chroma can be calculated from the color coordinates by using Pythagoras’ theorem:
A saturated (or brilliant) color is represented by a color point that is far away from the lightness axis. The color point of a pale (or dull, or pastel) color, a color of low saturation, is close to the L*-axis.
The views, opinions and technical analyses presented here are those of the author or advertiser, and are not necessarily those of ULProspector.com or UL. The appearance of this content in the UL Prospector Knowledge Center does not constitute an endorsement by UL or its affiliates.
All content is subject to copyright and may not be reproduced without prior authorization from UL or the content author.
The content has been made available for informational and educational purposes only. While the editors of this site may verify the accuracy of its content from time to time, we assume no responsibility for errors made by the author, editorial staff or any other contributor.
UL does not make any representations or warranties with respect to the accuracy, applicability, fitness or completeness of the content. UL does not warrant the performance, effectiveness or applicability of sites listed or linked to in any content.
Share this article:
Urinalysis (with sediment microscopy)
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
We remind you that independent interpretation of the results is unacceptable, the information below is for reference only.
Urinalysis (with sediment microscopy): indications for prescription, rules for preparing for the test, interpretation of the results and normal indicators.
Indications for testing
Complete urinalysis refers to routine laboratory tests aimed primarily at screening for diseases of the urinary system, since pathological processes in the kidneys and urinary tract affect the properties of urine.
This simple diagnostic test can detect diseases of an infectious and inflammatory nature, such as glomerulonephritis (inflammation of the renal glomeruli), pyelonephritis (inflammation of the renal pelvis), cystitis (inflammation of the bladder).
Microscopy of the urine sediment allows us to suspect an injury or heart attack of the kidney, urolithiasis, some neoplasms, amyloidosis of the kidneys (a systemic disease in which a specific insoluble protein is deposited in the kidneys, which disrupts the functioning of the organ).
In addition to diagnosing diseases of the kidneys and urinary tract, the results of a urinalysis with sediment microscopy can provide information about the general state of health.
Urine is formed by ultrafiltration of blood plasma through the glomeruli of the kidneys. With the development of various diseases, pathological metabolic products enter the blood, which are excreted from the body, including through the kidneys.
Preparation for the procedure
Preparation for the general urinalysis begins the day before the collection of biomaterial. Some foods, the amount of liquid you drink, taking medications and dietary supplements, intense physical activity can distort the results of the study.
The day before urine collection, avoid foods that can affect the color of urine: for example, beets and blueberries give the urine a reddish tint, if you eat a lot of carrots or carotene supplements, the color of urine can change to orange.
Alcohol, coffee, dietary supplements and strong tea are not recommended the day before urine collection. If possible, you should limit the intake of diuretic (diuretic) drugs. It is required to exclude serious physical exertion, as well as visiting baths, saunas.
Women who are menstruating are not recommended to give urine for analysis, since even a small amount of blood will significantly distort the result of the analysis.
Tell your doctor if you are taking any medications or if you have any invasive tests (eg, cystoscopy) before the test.
Method for collecting urine for general analysis
- It is necessary to prepare a disposable sterile container for collecting urine in advance (can be purchased at a pharmacy or taken from the INVITRO medical office).
- Before collecting urine, the vulva should be cleaned, and no antibacterial or disinfectant should be used. For children, the following rules must be followed: girls are washed from front to back (from the pubis to the coccyx) so that the bacteria that inhabit the intestines do not enter the urinary tract.
Soap is washed only on the skin, because if it gets on the mucous membranes, irritation, dryness and itching occur. In boys, the glans penis is fused with the foreskin (phymosis), so it is not recommended to forcibly open the glans penis, as this leads to trauma to the delicate tissue.
 It is only necessary to slightly pull the skin and rinse with water, while directing a stream of water into the opening of the urethra is unacceptable.
It is only necessary to slightly pull the skin and rinse with water, while directing a stream of water into the opening of the urethra is unacceptable. - For the general analysis, as a rule, collect the first morning portion of urine. First, a small amount of urine is released into the toilet, then, without interrupting urination, a container is placed and approximately 50 ml of urine is collected. In this case, it is necessary to ensure that the container does not touch the skin and mucous membranes.
- After collecting the urine, close the container tightly with a screw cap.
- Special urinals have been developed for newborns and infants. Urine squeezed out of a diaper or diaper should not be used - the results will be unreliable, since the diaper is a kind of filter for the microscopic elements of urine that are counted during the study.
- When testing during the day, it is not recommended to consume large amounts of water, tea, coffee or diuretics in order to stimulate urination.

The turnaround time for a urinalysis is usually 1 business day.
What can affect the results
Factors that may distort the result of the study:
- Violation of the hygiene procedures and urine collection technique.
- Drinking large or small amounts of water.
- Use of foods, drugs or supplements that change the color of urine.
- Menstruation.
- High blood pressure.
- Intense physical and psycho-emotional stress on the eve of urine collection.
- Visiting baths, saunas, hypothermia.
- Conducting invasive procedures on the urinary tract one week before the test.
You can submit a general urine test at the nearest INVITRO medical office. The list of offices where biomaterial is accepted for laboratory testing is presented in the "Addresses" section.
Urine examination includes the study of physical and chemical properties, as well as microscopy of the sediment.
Physical properties: amount, color, smell, transparency, relative density (specific gravity), urine reaction (pH).
Chemical properties: determination of protein, glucose, ketone bodies, urobilinogen, bilirubin, hemoglobin, nitrite, leukocyte esterase.
Microscopy: detection of erythrocytes, leukocytes, squamous, transitional and renal epithelial cells, cylinders, crystals, mucus, bacteria, fungi.
Normal
| Index | Result |
| Quantity | 50 ml |
| Color | Colorless, light yellow, straw yellow, yellow, amber yellow |
| Smell | Odorless or non-specific |
| Transparency | transparent |
| Relative density of urine (specific gravity) | 1003-1035 |
| Urine reaction (pH) | 5. 0-8.0 (in children under 1 month - 5.0-7.0) 0-8.0 (in children under 1 month - 5.0-7.0) |
| Protein | > 0.140 g/l |
| Glucose | > 2.8 mmol/l |
| Ketone bodies | > 1 mmol/l |
| Urobilinogen | > 34 mmol/l |
| Bilirubin | Not detected |
| Hemoglobin | Not detected |
| Leukocyte esterase | Not detected |
| Nitrites | Not detected |
| red blood cells | Up to 2 cells per field of view |
| Leukocytes | Up to 5 cells per field of view |
| Epithelium | Up to 5 squamous cells per field of view |
| cylinders | Not detected |
| crystals | Small amount of urates, calcium oxalates, amorphous phosphates or not detected |
| Slime | In a small amount |
| bacteria | Not detected |
| Fungi | Not detected |
Explanation of indicators
It should be remembered that a general urinalysis is a screening study, so its results can be used when prescribing other laboratory and instrumental examinations to clarify the diagnosis.
The color of urine depends on the concentration of substances dissolved in it and ranges from clear to amber yellow.
Under normal conditions, urine is colored by products of pigment metabolism (in particular, bilirubin): urochromes, urobilinoids and other substances. With an increase in the level of bilirubin in the blood, it enters the urine in greater quantities and gives it a rich brownish or even greenish-brown color. When erythrocytes (red blood cells), myoglobin (the main protein of muscle tissue) or hemoglobin (a protein contained in erythrocytes) enter the urine, its color changes to brown-red and takes on the appearance of "meat slops". Taking vitamins and preparations of the nitrofuran series can give urine a color from lemon yellow to orange. With a large number of leukocytes (white blood cells), the urine becomes milky (this condition is called pyuria).
Transparency. Urine is clear under normal conditions. Its turbidity can be caused by the presence of salts, crystals, cellular elements (erythrocytes, leukocytes).
Smell . Normally, urine has a slight non-specific odor. The appearance of an ammonia smell may be a sign of a bacterial infection, a peculiar fruity smell (“rotting apples”) appears with an increase in the concentration of ketone bodies (which most often indicates diabetes mellitus - a violation of glucose metabolism).
Urine relative gravity , or specific gravity, is determined using a urometer. The relative gravity of the urine gives an indication of the concentration capacity of the kidneys and the dilution function, which decrease, as does the relative gravity of the urine, in renal failure.
Urine reaction (pH) is a pH indicator that reflects the ability of the kidneys to maintain the acid-base balance of the body. The kidneys are involved in the excretion of hydrogen ions and bicarbonates, keeping the pH of the blood constant. The pH value of urine is greatly influenced by diet, metabolic characteristics, infectious and inflammatory processes in the kidneys and urinary tract.
Protein in urine is a significant marker in the diagnosis of diseases of the kidneys, urinary tract and cardiovascular system, it is also important in the diagnosis of preeclampsia - a severe complication of pregnancy. The appearance of protein in the urine is called proteinuria. Normally, urine does not contain protein, because the kidney filter prevents the release of protein molecules from the blood into the urine. There are several causes of proteinuria.
- Prerenal causes: intense physical and psycho-emotional stress, heart failure, hypertension, fever, preeclampsia during pregnancy, nephroptosis, forced standing for a long time (often in hairdressers, surgeons, military personnel), injuries, violation of the protein composition of blood plasma.
- Renal causes: glomerular disease (glomerulonephritis and glomerulopathy), tubular disease, nephrosclerosis.
- Postrenal causes: infectious and inflammatory processes in the urinary tract, neoplasms.

Urine glucose. The appearance of glucose in the urine depends on its concentration in the blood. Normally, glucose is completely reabsorbed from primary urine into the bloodstream if its concentration in the blood has not reached the "renal threshold" - 8.8-10.0 mmol / l. An increase in the level of glucose in the urine is possible due to a number of physiological reasons: errors in the diet (abuse of sweet foods, especially on the eve of collecting biomaterial), prolonged starvation, stress.
The appearance of glucose in the urine is a signal indicating the pathology of the kidneys, endocrine system, side effects of drugs, poisoning, complicated pregnancy.
Ketone bodies are non-specific. The appearance of an increased amount of ketone bodies in the urine is the result of an accelerated fat metabolism or a reduced carbohydrate metabolism. Most often, an increase in their level is observed during starvation, fever, vomiting, alcohol intoxication and diabetes mellitus.
Urobilinogen in urine increases in diseases of the intestines, liver, in hemolytic conditions (destruction of red blood cells).
Bilirubin appears in the urine with liver pathologies, infectious diseases and pigment metabolism disorders.
Hemoglobin is determined with a large number of erythrocytes in the urine, with myositis, extensive injuries of muscle tissue, thrombosis of muscle vessels.
Nitrite in the urine is detected by the activation of pathogenic microflora in the urinary system.
An increase in the number of erythrocytes is observed in the following cases:
- Inflammatory diseases of the kidneys and urinary tract of infectious and non-infectious origin (glomerulonephritis, pyelonephritis, nephritis, cystitis, prostatitis, tuberculosis).
- Urolithiasis.
- Traumatic injury to the kidneys and urinary tract.
- Fever.
- Arterial hypertension involving the renal vessels.

- Various disorders of blood coagulation (with hemophilia, thrombocytopenia, overdose of anticoagulants).
- Poisoning with derivatives of benzene, aniline, snake venom, poisonous mushrooms, with intolerance to anticoagulant therapy.
- Tumor diseases of the genitourinary system.
The presence of leukocytes in the amount of more than five cells per field of view is noted in the following cases:
Epithelium . There are cells of flat, transitional and renal epithelium. A large amount of epithelium indicates increased desquamation of cells of the mucous membrane of the urinary tract when they are traumatized (by a stone, during an inflammatory process).
Cylinders are formed in the tubules of the kidneys and allow you to determine the level of damage to them. Most often found in glomerulonephritis.
Most often found in glomerulonephritis.
Crystals of are detected in salt sediment at a certain pH of the urine. Most often (though not always) occur in patients with urolithiasis.
Mucus can normally be found in the urinary sediment in small quantities. An increase in the content of mucus can be associated both with an inflammatory process in the urinary tract, and with errors made when collecting urine for research.
Bacteria and fungi are normally not found in the urinary sediment. Their presence indicates the presence of an infectious process in the kidneys and urinary tract or errors made when collecting biomaterial for research.
In case of deviation from the norm of indicators of the general analysis of urine, the following instrumental examinations and laboratory tests can be additionally prescribed:
- Complex ultrasound of the urinary system (kidneys, ureters, bladder).
- Comprehensive ultrasound of the abdominal organs (liver, gallbladder, pancreas, spleen) for suspected diseases of the liver, gallbladder, etc.

- Study of biochemical blood test parameters (total protein, protein fractions, C-reactive protein, ALT, AST, LDH, GGT, total and direct bilirubin, cholesterol, creatinine, glucose, electrolytes: potassium, sodium, chlorine, calcium).
- Fasting blood glucose test, oral glucose tolerance test, glycated hemoglobin test to diagnose diabetes mellitus.
- Urine culture for microflora and determination of sensitivity to antimicrobial drugs.
- Urine culture and susceptibility to extended spectrum antimicrobials.
If you change the parameters of the general analysis of urine, you may need to consult a general practitioner
, a pediatrician or a general practitioner, as well as a
urologist
, a nephrologist,
endocrinologist
.
Sources:
- Children's Nephrology: Textbook / ed. P.V. Shumilova, E.K. Petrosyan, O.L. Chugunova. - M.: MEDpress-inform, 2018. - 616 p.: ill.
- Grebenev A.L. Propaedeutics of internal diseases: Textbook. – 5th ed., revised. and additional - M.: Medicine, 2001. - 592 p.: ill.
- Danilova L.A. Analyzes of blood, urine and other biological fluids at various age periods. - St. Petersburg: SpetsLit, 2014. - 111 p.
- cdp.dt.mvd.rf.
- www.ncbi.nlm.nih.gov
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
VACUETTE 9 vacuum tube color code0001
March 2, 2020
In the modern world, more and more attention is paid to laboratory research and the quality of their conduct.
An important component of any laboratory research is a test tube. She participates in all laboratory stages, starting with taking the biomaterial from the patient. The results of research depend on the quality of the test tube, its contents (reagent) and the stability of the vacuum.
What most of all pays attention to any person who sees the test tube? Bright cap color! This is not just a design decision, it is the convenience of nurses and laboratory assistants. These requirements are reflected in GOST ISO 6710-2011 “Disposable containers for collecting venous blood samples. Technical requirements and test methods" and GOST R 53079.4-2008 “Laboratory clinical technologies. Ensuring the quality of clinical laboratory research. Part 4. Rules for conducting the preanalytical stage.
So, what do these bright caps mean. Each tube has a certain reagent or does not have it, which is also coded in a certain color. Let's take a closer look at each color and reagent.
This tube contains a buffered solution of sodium citrate in possible percentages of 3.2 and 2.8. This type of tubes is used to study the hemostasis system (coagulogram). This type of study includes such indicators as: APTT, prothrombin, fibrinogen, thrombin time and others.
Also, tubes with a blue cap can contain a CTAD reagent. This reagent is used for the same studies, but it is used in the study of patients receiving anticoagulant therapy. The composition of the reagent includes buffered sodium citrate, theophylline, adenosine and dipyridamole.
These test tubes are used for the study of blood serum. Blood serum, unlike plasma, does not contain fibrinogen, therefore, in order to obtain a serum sample, it is necessary to activate the sample clotting process.
In test tubes with a red cap, this process is activated due to silicon dioxide (SiO2) deposited on the inner walls in the form of microparticles. In addition to the reagent, this type of tube may contain a separation gel. It creates a reliable barrier between the clot and serum, which is important during sample storage and transportation. Test tubes with clotting activator are used for research in: biochemistry, immunology, microbiology, serology and others.
It creates a reliable barrier between the clot and serum, which is important during sample storage and transportation. Test tubes with clotting activator are used for research in: biochemistry, immunology, microbiology, serology and others.
Unlike test tubes with a red cap, they are used to obtain plasma.
They must contain a reagent that blocks the clotting process. Tubes with green caps contain the anticoagulant heparin (sodium heparin, lithium heparin, ammonium heparin). This type of tube may also contain a gel for greater sample stability. It creates a reliable barrier between plasma and shaped elements during transportation. Test tubes with anticoagulant can be used for such studies as: electrolyte composition of the blood, blood gases, blood alcohol content.
The reagent contained in these test tubes binds calcium ions and blocks the clotting process. The reagent consists of ethylenediamineacetic acid (EDTA). EDTA-k2 or EDTA-k3 is applied to the inner walls of the test tube. These test tubes have been reassigned for hematological studies (qualitative and quantitative composition of blood). For molecular genetic studies and determination of viral load, test tubes with EDTA and separation gel are used.
These test tubes have been reassigned for hematological studies (qualitative and quantitative composition of blood). For molecular genetic studies and determination of viral load, test tubes with EDTA and separation gel are used.
This tube contains the KEDTA reagent and aprotinin (a stable protein isolated from bovine lungs), an inhibitor of tissue and serum proteolytic enzymes (trypsin, hemitripsin, plasmin, kallikrein). This reagent helps to stabilize unstable and problematic analytes (eg some hormones).
6. Tube with gray cap (with different reagents: lithium heparin and monoiodoacetate or sodium fluoride and potassium oxalate).
Special tubes for testing glucose with several reagent options: monoiodoacetate and lithium heparin, sodium fluoride and potassium oxalate, sodium fluoride and CzEDTA. Due to the fact that the reagent contains not only an anticoagulant, but also a glucose level stabilizer, the sample can remain stable for up to 48 hours at room temperature.
7. Tubes with yellow cap (with citric acid, sodium citrate, dextrose).
The combination of reagents in test tubes of this type helps for a long time (within 21 or 35 days) to maintain the stability of samples at a temperature of 1-6 degrees. The composition of the reagent includes (ACD-A, ACD-B) - citric acid, sodium citrate, dextrose; (CPDA) - citric acid, sodium phosphate, dextrose, adenine.
Used to determine the ESR and as part of the reagent have 3.2% sodium citrate.
This material is for informational purposes only and should not be used as a tutorial.
omb.ru
06.10.2022 10:13
The role of ferritin in the diagnosis and differentiation of anemia
Anemia is one of the most common diseases diagnosed in more than 1.62 billion people (about 25% of the world's population)..
03.10.2022 09:50
One way to reduce the intensity of pain during blood sampling in newborns
Pain in newborns is a key factor, since during this period the sensory area is the most active area of their brain.